-
Board-Certified
Fellowship-Trained
Physical Medicine
& Rehabilitation
Minimally Invasive Surgery
How minimally invasive surgery gets you home the same day for a faster recovery
 In traditional spine surgery, the surgeon makes a three-inch incision to access a herniated disc, which can disrupt ligaments and tendons making recovery longer and more painful.
In traditional spine surgery, the surgeon makes a three-inch incision to access a herniated disc, which can disrupt ligaments and tendons making recovery longer and more painful.
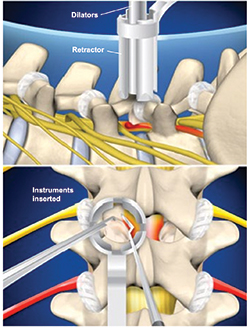
By contrast, spine surgeon Dr. Michael Kilburn at South Carolina Spine Center uses special tools called tubular retractors. A small half-inch incision is made and the surgeon is to access the spine through instruments inserted through the tube. A series of dilators of increasing size are carefully guided down through muscles and soft tissue. The surgeon slides the tubular retractor to create a channel that doesn’t disrupt muscle and soft tissue. This channel enables the trained spine surgeon to access the vertebra and nerve root with minimal disruption to the muscles and tissues in the back. The problematic bone or tissue is then removed from around the nerve root, relieving the pain symptom.
New minimally invasive spine surgery techniques can include the following:
MIS Lumbar Microdiscectomy/Laminectomy
A minimally invasive lumbar discectomy is when a herniated disc is removed in the lower back that pinches a nerve that may cause severe leg pain, numbness, or weakness. This procedure is done by making a small 1-inch incision over the herniated disc and inserting a tubular retractor. Then the surgeon removes a small amount of the lamina bone that allows the surgeon to view the spinal nerve and disc. Once the surgeon can view the spinal nerve and disc, the surgeon will retract the nerve, remove the damaged disc, and replaces it with bone graft material.
MIS Posterior Cervical Discectomy
A minimally invasive posterior cervical discectomy is when a herniated disc is removed in the back of the neck that pinches a nerve that may cause severe arm pain, numbness or weakness. This procedure is done by making a small 1-inch incision over the herniated disc and inserting a tubular retractor. Then the surgeon removes a small amount of the lamina bone that allows the surgeon to view the spinal nerve and disc. Once the surgeon can view the spinal nerve and disc, the surgeon will retract the nerve and remove a portion of the damaged disc, which decompresses the nerve. (If a fusion is required, the surgeon will replace the disc with a bone graft. This procedure would then be called a MIS Posterior Cervical Discectomy & Fusion.)
MIS Lumbar Fusion
A minimally invasive lumbar fusion can be performed the same way as traditional open lumbar fusion, either from the back, through the abdomen, or from the side.
Lateral interbody fusion
A lateral interbody fusion, often used to treat spondylolysis, degenerative disc disease and herniated discs, is performed by removing a disc and replacing it with a spacer that will fuse with the surrounding vertebra. The procedure is completed on the side of the body in order to reduce the effect on the nerves and muscle of the back.
 Posterior cervical microforaminotomy
Posterior cervical microforaminotomy
A PCMF is performed to help relieve pressure and discomfort in the spine by making a small incision in the back of the neck and removing excess scar tissue and bone graft material.
Anterior cervical discectomy
An anterior cervical discectomy is used to reduce pressure or discomfort in the neck by removing a herniated disc through a small incision in the front of the neck. The space is then filled with bone graft material and plates or screws may be used to increase stability.
How the patient benefits from minimally invasive spine surgery
- Tiny incision covered by a small bandage.

- Less disruption to tissues and muscles
- Patient is home later the same day.
- Less pain after surgery & quicker recovery.
- Less blood loss and need for donated blood.
- Fewer complications from a short incision.
- Less painful rehab
- Quicker return to activity
Minimally Invasive Surgery Overview
Several weeks of recovery may be required for traditional "open" spine surgery as it may involve a three-inch long incision, in which muscles and tissues are separated for optimal access to the injury site. The surgery usually results in trauma to surrounding tissues and some blood loss. Because of this the affected tissues and muscles need adequate healing time.
In contrast, South Carolina Spine Center spine surgeons use state of the art minimally invasive techniques and instrumentation to help patients recover in a shorter period of time and allow for a quicker return home.
Illustrations Copyright © Viewmedica,
used by permission.
Innovative developments in minimally invasive techniques have pioneered better ways for the surgeon to access the spine, moreover making the recovery process more seamless. In minimally invasive spine surgery, a smaller incision is made, sometimes only a half-inch in length. The surgeon inserts special surgical instruments through these tiny incisions to access the damaged disc in the spine. Entry and repair to the damaged disc or vertebrae is achieved without harming nearby muscles and tissues when using minimally invasive techniques.
Minimally invasive spine surgery requires extensive training and experience to master use of the tools, but there is tremendous benefit for the patient. The incision is shorter, which means you aren't cutting through as much muscle and tissue to get access to the damaged area of the spine.
Unlike many other spine care providers, the spine patients who undergo minimally invasive surgery with South Carolina Spine Center can often have their surgery on an outpatient basis and be home later the same day. Recovery in one's own home can be more comfortable than staying in a hospital bed.
Physician Biographies
-
 Karl Boellert, MD
Karl Boellert, MD -
 Mathew Gowans, MD
Mathew Gowans, MD- Board-Certified
Physical Medicine
& Rehabilitation
- Board-Certified
-
 Michael P.B. Kilburn, MD
Michael P.B. Kilburn, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
-
 Sumeer Lal, MD
Sumeer Lal, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
-
 John Cole, MD
John Cole, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
Back to Life Journal

Home Remedy Book

![]() Website Design & Educational Content © Copyright 2023 Prizm Development, Inc.
Developing Centers of Excellence for Better Healthcare.
Website Design & Educational Content © Copyright 2023 Prizm Development, Inc.
Developing Centers of Excellence for Better Healthcare.
Prizm is the most experienced developer of spine and orthopedic centers in the U.S. with content-rich educational web sites for physicians.
