-
Board-Certified
Fellowship-Trained
Physical Medicine
& Rehabilitation
Artificial disc replacement at South Carolina Spine Center
While most back or neck pain is caused by either a muscle or ligament strain, which never requires surgery, some people can herniate a disc which can require spine surgery to relieve the symptoms. In some cases, the presence of a herniated disc can imply that the patient is at risk of degenerative disc disease, meaning that they may experience herniations at other levels as well.
Consequently, those who have a herniated disc at one level in their low back or neck, can sometimes have additional herniated discs appear in the future. For these people, the newest FDA-approved artificial discs available now can be of great benefit.
 The role of the healthy disc
The role of the healthy disc
A healthy disc acts like a shock absorber in between the bony vertebrae of the spine, enabling the spine to rotate. The disc itself resembles a jelly donut. If the disc is compressed or ruptures (from trauma or the stress of lifting something heavy) the jelly center, called the nucleus pulposus, can break through the wall of the disc.
This disc nucleus can then press on nearby spinal nerves causing radiating pain and numbness. Herniated discs in the low back typically cause radiating pain or numbness or weakness in a leg or foot. Herniated discs in the neck conversely cause radiating pain or numbness or weakness into an arm or hand.
While a person can use watchful waiting for three to six months for radiating pain into a leg or arm, that is not the case when the symptom is numbness or weakness in a leg or arm. This symptom is called “neurological deficit” and signals that the herniated disc is pressing on a nerve root off the spinal cord.
Those with symptoms of numbness or weakness in a foot or hand need to be seen by a spine surgeon within 48 hours. Left untreated these symptoms can become permanent and lifelong.
Another emergency symptom that appears less frequently is “cauda equina,” where the person experiences loss of control of bowel or bladder because of a herniated disc in the low back. A person with this symptom needs to go immediately to an Emergency Room. If these symptoms are not treated promptly, the nerve root can be permanently damaged, much like a car parked in the driveway for several days on a garden hose. Even if the car is moved, the hose may be permanently crimped.

Fixing a herniated disc
When a disc herniates, it’s important to understand that the surgeon cannot repair the disc wall. The surgeon instead removes the part of the disc that is pressing on a nearby nerve root. If the disc has been compressed, the surgeon must restore the disc space between the vertebrae by inserting a spacer between the two vertebrae.
The spacer could be a piece of bone harvested from the patient’s own hip bone, or a sterilized piece of cadaver bone from a bone bank. The process of removing the damaged disc and inserting the bone spacer is called a spinal fusion.
Each year in the U.S., more than 200,000 spinal fusion surgeries are performed to relieve pain or numbness caused by damaged discs in the low back and neck.
While the intent of a spinal fusion is to relieve the symptoms of pain or numbness, the downside of spinal fusion surgery is that it causes two vertebrae to become locked in place. This in turn puts additional stress on discs above and below the affected area, which can cause additional herniations above and below the fusion level.
How an artificial disc works
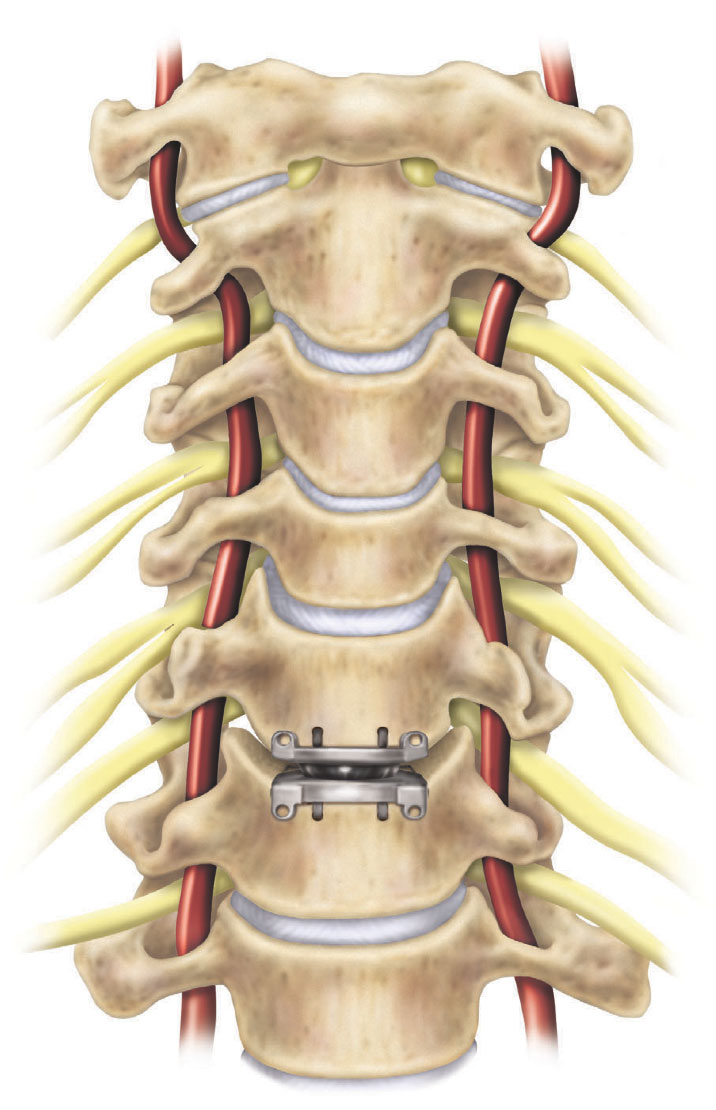
An artificial disc replacement is intended to duplicate the rotation of a normal, healthy disc and retain motion in the spine, which lessens the risk of herniation at the other disc levels.
Artificial discs have been used in Europe since 1987. Because of the FDA’s rigorous approval process, artificial disc use in the U.S. did not begin until 2004.
Future development of new artificial discs attempt to not only mimic and reproduce the function of the normal disc by providing rotational movement but also up and down shock absorption. Other issues in artificial disc design try to take into account the possibility of revision and replacement surgery if an artificial disc wears out over 10 to 20 years.
 Artificial discs for the low back
Artificial discs for the low back
There is a big difference in the artificial discs used in the lumbar (low back) area, and the artificial discs used in the cervical (neck) area. Because of the weight of the body and the rotational stress that the trunk places on discs in the low back (lumbar) area, more stress is placed on artificial discs in the lumbar area than in the neck (cervical) area, which only supports the weight of the head.
A second issue relates to the ease of the artificial disc surgery and any necessary revision surgery to replace a worn out artificial disc. Because the surgeon must access the front of the spine, an incision is made in the abdomen for lumbar discs. This can require navigating around internal organs to access the discs at the front of the spine in the low back. Consequently revision surgery related to replacing a worn out lumbar artificial disc is far more complicated than neck surgery.
Because of these issues, many spine surgeons are cautious about using the current artificial discs in the low back area. Some spine surgeons feel that the disc technology is still evolving and improving.
About the Medtronic Prestige LP Cervical Disc
At South Carolina Spine Center in Greenwood, SC, the spine surgeons use the Medtronic Prestige LP cervical disc for artificial disc replacement in the neck. The Prestige artificial disc was one of the first artificial discs to be approved by the U.S. Food & Drug Administration (FDA) for 2 levels in the neck.
The Prestige LP cervical disc has two components that the spine surgeon installs between the vertebrae to replace the herniated disc. The artificial disc is constructed with a mixture of metals commonly used in spine surgery such as titanium ceramic composite and a ceramic material, titanium carbide. The artificial disc preserves range of motion in the neck by allowing flexion, extension, side bending, and rotation and preserving the correct height and curvature of a natural disc.
Medtronic reported a 7-year study where the 2-level Prestige LP Cervical Disc was compared to 2-level anterior cervical discectomy and fusion. The study concluded:
- The 2-level Prestige patients showed greater rates in overall success — 78.6 percent — compared to the patients treated with 2-level ACDF — 62.7 percent.
- The Prestige disc patients showed a neurological success rate of 91.6 percent compared to the patients treated with two-level ACDF who saw a neurological success rate of 82.1 percent.
- The Prestige disc patients exhibited greater success rates in patient-reported outcomes, including Neck Disability Index — 87.0 percent — as compared to the 75.6 success rate that patients treated with two-level ACDF experienced.
- The artificial disc lowered the risk of a second surgery. Around 4.2 percent of Prestige patients needed second surgeries, compared to 14.7 percent of 2-level ACDF patients.
Another recent study presented at the North American Spine Society (NASS) which is the nation’s largest group of spine surgeons, concluded that the use of an artificial disc in the neck reduced the incidence of “adjacent segment disease”, meaning that it reduced the likelihood that other discs in the neck would herniate.
In the neck, it is important to remember that there are 7 vertebral levels (C-1 throught C-7) and only 6 discs between those levels. If two discs are herniated and subsequently fused and locked, that only leaves 4 discs to provide any motion of the neck. Consequently, over time those remaining discs are going to have extreme loading and higher risk of herniation. This then would completely lock up the neck and prevent any motion.
Consequently, with this new research, artificial disc replacement in the neck has now become widely accepted over the last few years as the new standard of care for herniated discs in the neck.
While there are many FDA-approved artificial disc options in the spine surgery field, the spine surgeons at South Carolina Spine Center at Self Regional Healthcare believe that there are significant patient benefits to selecting a single artificial disc system and becoming extremely proficient in that specific system. By focusing on one system it will improve clinical outcomes from artificial disc replacement surgery.
Who qualifies for cervical artificial disc replacement?
Not everyone qualifies for an artificial disc as some symptoms are not appropriate for the device. Typically, the patients who are candidates for an artificial disc replacement in the neck include the following:
- You are an adult (between 21 and 78 years old) and your spinal bones are mature and of good quality.
- You have arm pain and/or symptoms like weakness, numbness or tingling.
- You have two diseased cervical discs next to each other between level C3 and level C7 that your doctor has determined require surgery.
- You have tried at least six weeks of non-surgical treatment and still have the same symptoms or are getting worse even with the other treatments.
SUMMARY: Pros and cons of the artificial disc
Benefits of the artificial disc:
- Retains motion of the vertebrae.
- Prevents damage to other levels.
- No bone graft required.
- Quicker recovery.
- Less painful surgery than a fusion.
- Less blood loss during surgery.
Spine surgeons may be cautious about artificial discs because:
- Wear and tear on artificial disc can require revision surgery in 10 to 20 years which can be complex.
- Disc implants only address rotational forces, not the up and down shock absorbing of the natural disc.
- Overweight people can wear out a lumbar disc prematurely.
- Newer artificial discs are in development that may be better.
Physician Biographies
-
 Karl Boellert, MD
Karl Boellert, MD -
 Mathew Gowans, MD
Mathew Gowans, MD- Board-Certified
Physical Medicine
& Rehabilitation
- Board-Certified
-
 Michael P.B. Kilburn, MD
Michael P.B. Kilburn, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
-
 Sumeer Lal, MD
Sumeer Lal, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
-
 John Cole, MD
John Cole, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
Back to Life Journal

Home Remedy Book

![]() Website Design & Educational Content © Copyright 2023 Prizm Development, Inc.
Developing Centers of Excellence for Better Healthcare.
Website Design & Educational Content © Copyright 2023 Prizm Development, Inc.
Developing Centers of Excellence for Better Healthcare.
Prizm is the most experienced developer of spine and orthopedic centers in the U.S. with content-rich educational web sites for physicians.
