-
Board-Certified
Fellowship-Trained
Physical Medicine
& Rehabilitation
Kyphosis
Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
Overview
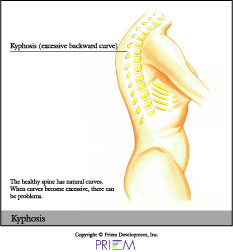
Kyphosis and lordosis are types of spinal deformities. While slight
curvature of the spine is normal and healthy, there are some cases
where it is over-pronounced and can cause both cosmetic deformity and
health risks. When the spine curves inward too much in the low back,
it is called lordosis. When the spine in the shoulder blade or mid-spine
area has too much forward curve, or too much of a hump, it is called
kyphosis. Kyphosis most often occurs in the thoracic area of the spine.
[top]
Causes
Some people are born with kyphosis when there is a naturally occuring abnormality in the spine. Kyphosis can also be an acquired condition. Teenagers in particular may develop kyphosis due to bad posture, especially girls between the ages of 12 and 15. Adolescent kyphosis is called Scheuermann's disease.
Compression fractures are often linked to the development
of many cases of adult kyphosis, because they cause vertebrae to become
wedged, reducing the amount of space between each vertebra. These fractures
can occur as the result of degenerating discs, arthritis, osteoporosis
and spondylolisthesis. Individuals with osteoporosis may develop kyphosis
due to a weakening and compression in the vertebrae. Kyphosis in these
individuals is treated with aggressive anti-osteoporosis action to
prevent further bone weakening.
[top]
Symptoms
 The symptoms of kyphosis are similar to those of scoliosis. These include
uneven shoulders, chest, hips, shoulder blades, waist, or a tendency
to lean to one side. In other cases, there are no visible symptoms.
To diagnose a person with scoliosis, have them touch their toes.
If either one or both shoulder blades are prominent, the waist is
shifted or ribs are uneven, kyphosis may be present. Kyphosis is
also called “hunchback” because of the hunched over appearance
often seen in patients. Other symptoms include fatigue and difficulty
breathing.
The symptoms of kyphosis are similar to those of scoliosis. These include
uneven shoulders, chest, hips, shoulder blades, waist, or a tendency
to lean to one side. In other cases, there are no visible symptoms.
To diagnose a person with scoliosis, have them touch their toes.
If either one or both shoulder blades are prominent, the waist is
shifted or ribs are uneven, kyphosis may be present. Kyphosis is
also called “hunchback” because of the hunched over appearance
often seen in patients. Other symptoms include fatigue and difficulty
breathing.
[top]
Diagnosis
Outlined below are some of the diagnostic tools that your physician may use to gain insight into your condition and determine the best treatment plan for your condition.
Medical history: Conducting a detailed medical history helps the doctor better understand the possible causes of your back and neck pain which can help outline the most appropriate treatment.
Physical exam: During the physical exam, your physician will try to pinpoint the source of pain. Simple tests for flexibility and muscle strength may also be conducted.
X-rays are usually the first step in diagnostic testing methods. X-rays show bones and the space between bones. They are of limited value, however, since they do not show muscles and ligaments.
MRI (magnetic resonance imaging) uses a magnetic field
and radio waves to generate highly detailed pictures of the inside
of your body. Since X-rays only show bones, MRIs are needed to visualize
soft tissues  like discs in the spine. This type of imaging is very
safe and usually pain-free.
like discs in the spine. This type of imaging is very
safe and usually pain-free.
CT scan/myelogram: A CT scan is similar to an MRI in that it provides diagnostic information about the internal structures of the spine. A myelogram is used to diagnose a bulging disc, tumor, or changes in the bones surrounding the spinal cord or nerves. A local anesthetic is injected into the low back to numb the area. A lumbar puncture (spinal tap) is then performed. A dye is injected into the spinal canal to reveal where problems lie.
Electrodiagnostics: Electrical testing of the nerves and spinal cord may be performed as part of a diagnostic workup. These tests, called electromyography (EMG) or somato sensory evoked potentials (SSEP), assist your doctor in understanding how your nerves or spinal cord are affected by your condition.
Bone scan: Bone imaging is used to detect infection,
malignancy, fractures and arthritis in any part of the skeleton.
Bone scans are also used for finding lesions for biopsy or excision.
Discography is used to determine the internal structure of a disc. It is performed by using a local anesthetic and injecting a dye into the disc under X-ray guidance. An X-ray and CT scan are performed to view the disc composition to determine if its structure is normal or abnormal. In addition to the disc appearance, your doctor will note any pain associated with this injection. The benefit of a discogram is that it enables the physician to confirm the disc level that is causing your pain. This ensures that surgery will be more successful and reduces the risk of operating on the wrong disc.
Injections: Pain-relieving injections can relieve back pain and give the physician important information about your problem, as well as provide a bridge therapy.
[top]
Treatment
When treating kyphosis, the cause of the disease must first be considered.
Some cases require surgery early on, while other times, bracing and
physical therapy may be the best course of action. Although bracing
can help reduce pain symptoms, it is less successful at fixing the
underlying problem of a curved spine, especially in adults. Strengthening
and stretching programs can be successful at reducing symptoms. Swimming
and other low-impact forms of exercise are beneficial. In cases which
require surgical intervention, the goal is to reduce the curvature
and relieve pain and discomfort over a long period of time.
[top]
FAQs
When is surgery necessary to treat kyphosis?
Surgery is always treated as a last resort, while more conservative methods are tried first. In general, surgery is considered when the curve exceeds 75 degrees. Other cases in which surgery may be recommended are for those suffering from chronic pain and/or a rapidly progressive curve.
How can I prevent kyphosis?
Strengthening the back muscles can help prevent poor posture, which
can lead to kyphosis. Osteoporosis, which can also cause kyphosis,
can be prevented by getting enough calcium and vitamin D, exercising
and strength training regularly.
[top]
Physician Biographies
-
 Karl Boellert, MD
Karl Boellert, MD -
 Mathew Gowans, MD
Mathew Gowans, MD- Board-Certified
Physical Medicine
& Rehabilitation
- Board-Certified
-
 Michael P.B. Kilburn, MD
Michael P.B. Kilburn, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
-
 Sumeer Lal, MD
Sumeer Lal, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
-
 John Cole, MD
John Cole, MD-
Board-Certified
Fellowship-Trained
Spinal Neurosurgeon
-
Board-Certified
Back to Life Journal

Home Remedy Book

![]() Website Design & Educational Content © Copyright 2023 Prizm Development, Inc.
Developing Centers of Excellence for Better Healthcare.
Website Design & Educational Content © Copyright 2023 Prizm Development, Inc.
Developing Centers of Excellence for Better Healthcare.
Prizm is the most experienced developer of spine and orthopedic centers in the U.S. with content-rich educational web sites for physicians.